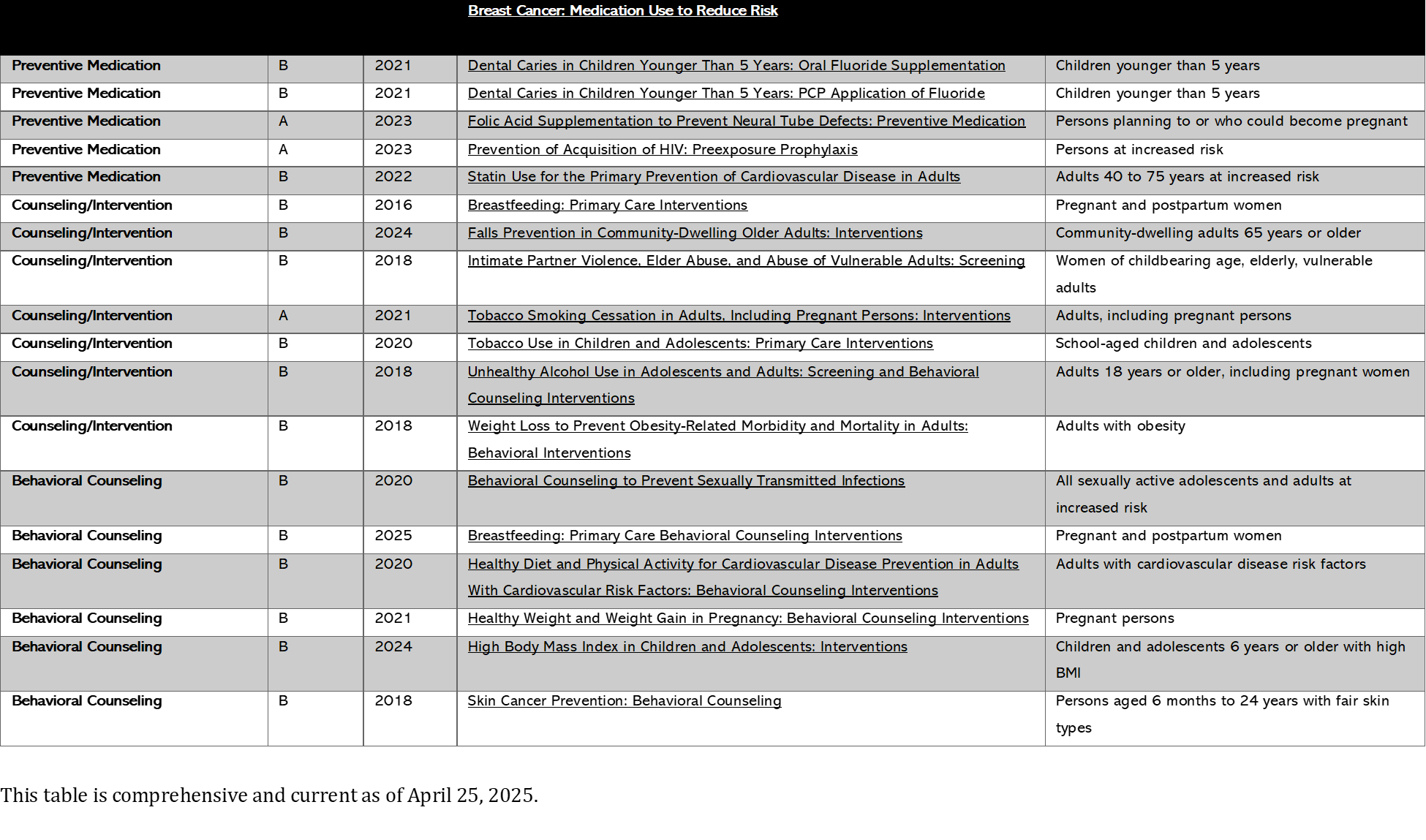
Prevention
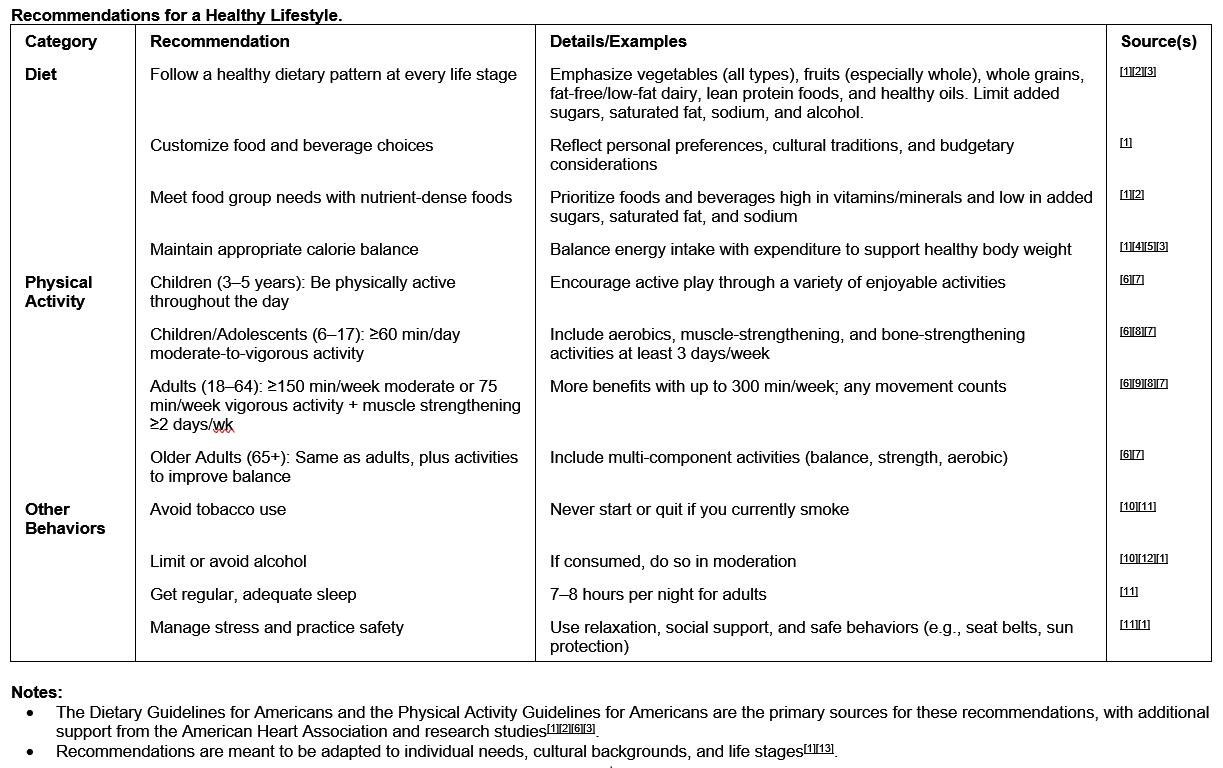
Top of PageBelow is a comprehensive list of preventable health conditions and accidents in the United States, categorized by type, with evidence-based prevention strategies. Sources include CDC guidelines and peer-reviewed public health recommendations.
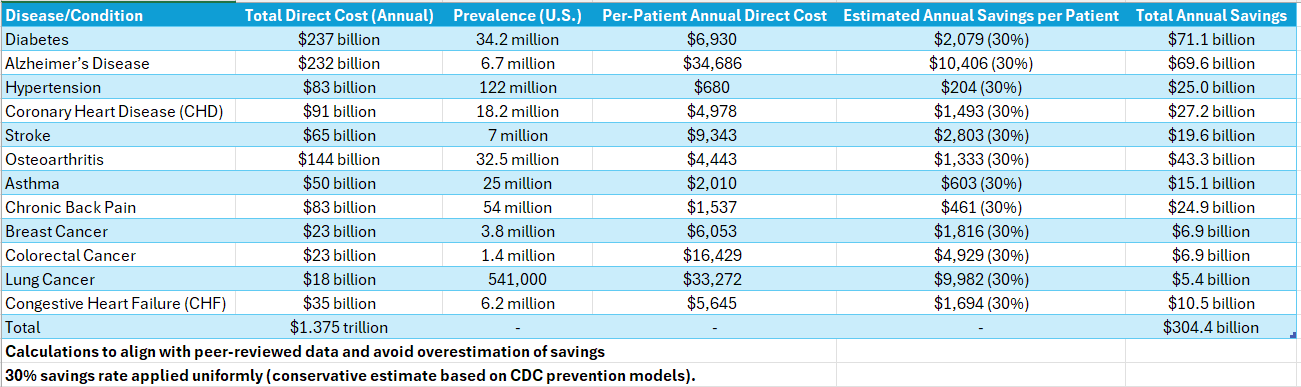
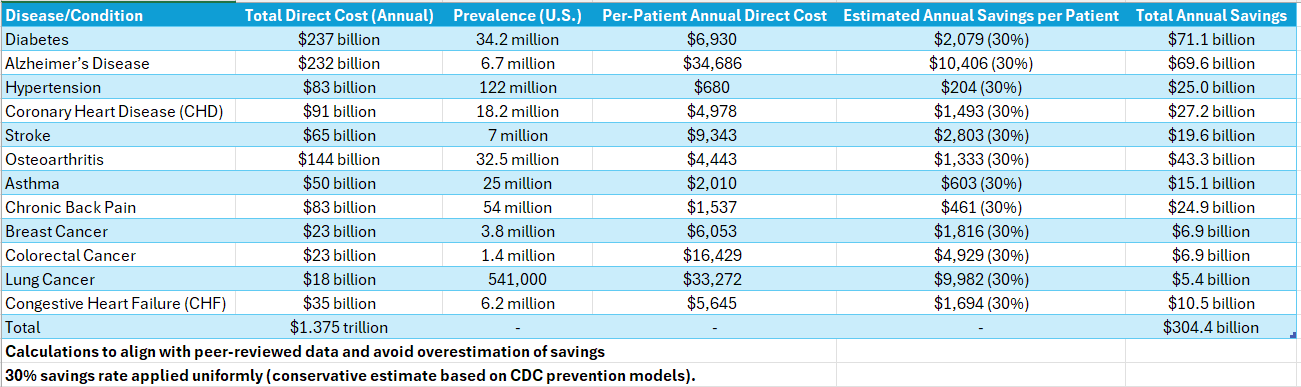
Estimated potential savings if an individual were to follow recommended prevention actions in the particular disease.
Note: For demonstration purposes only. Not an official estimate from an authoritative source. AI generated.
Summary: Non-vaccine preventable diseases cost the U.S. $1.375 trillion annually in direct healthcare expenses. Implementing prevention strategies (e.g., lifestyle changes, early diagnosis) could save $304.4 billion/year, with diabetes, Alzheimer’s, and heart disease offering the largest savings opportunities.
Summary Report of the estimation (pdf).
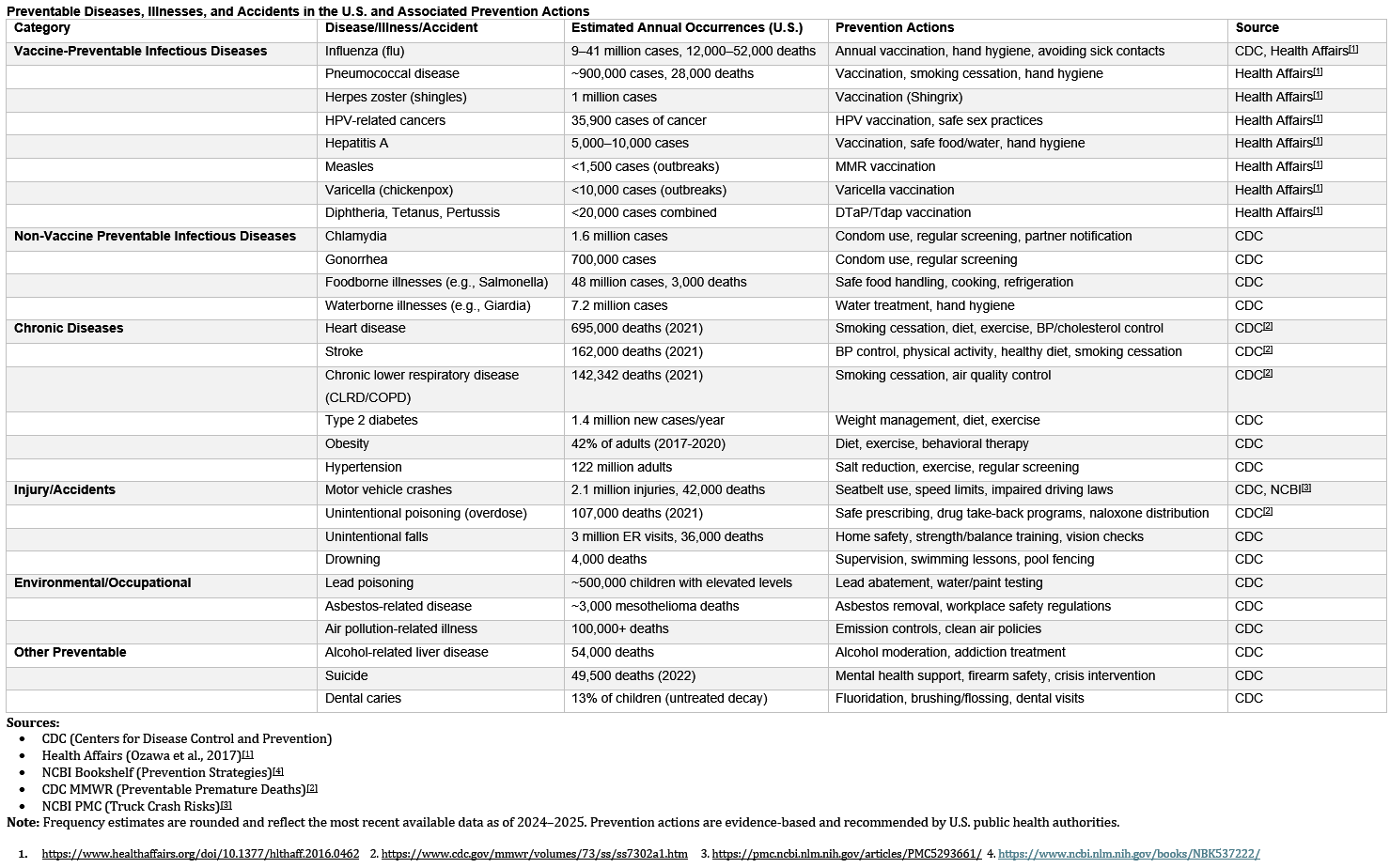
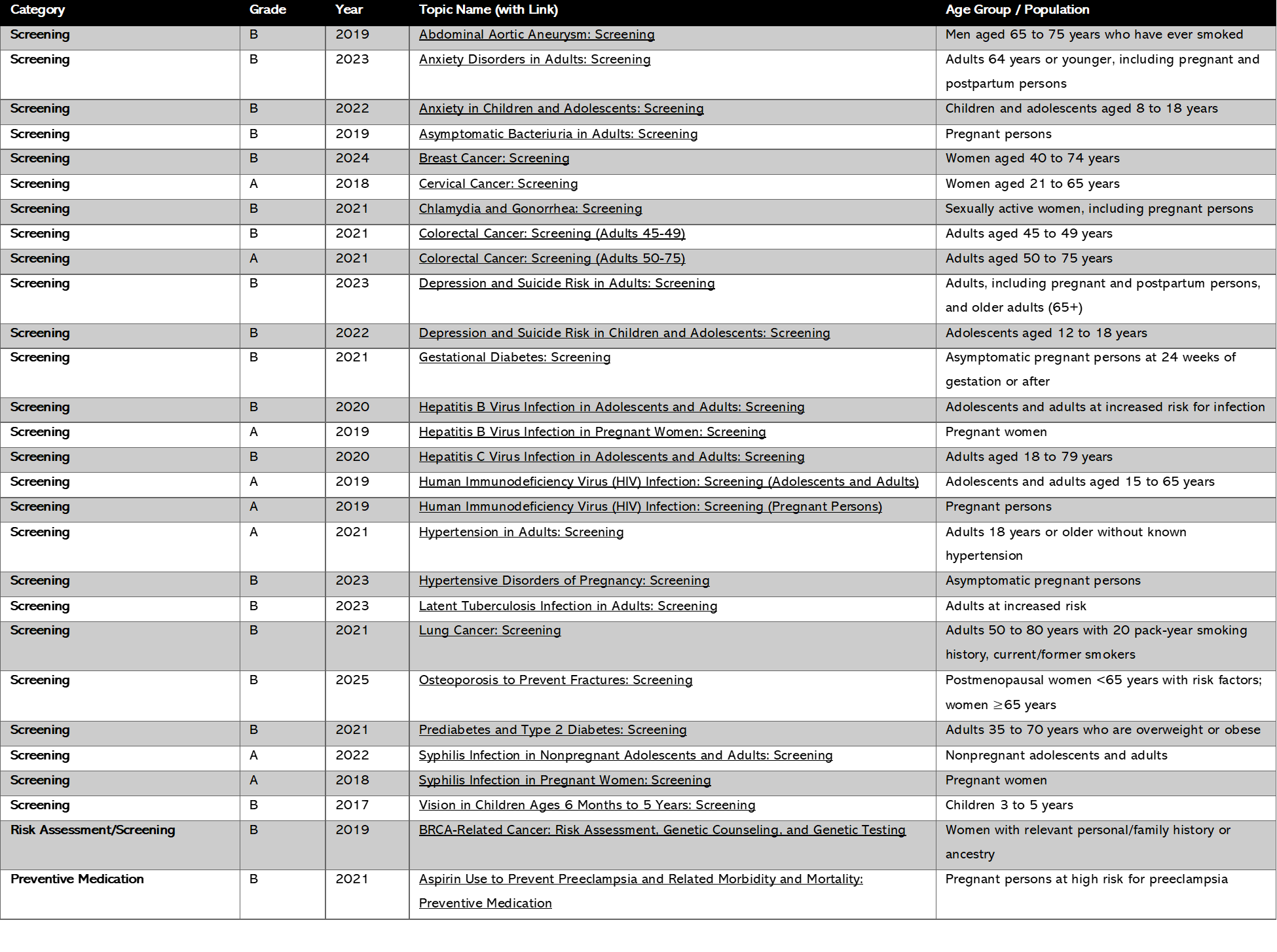
U.S. Preventive Services Task Force: A listing of all the Recommendations with a grade of either A or B. A and B grade recommendations are services that the Task Force most highly recommends implementing for preventive care.
Vaccines for: Your Children Adults
MyHealthfinder: See which screening tests and vaccines you or your loved ones need to stay healthy.
Find free or low-cost preventive care. OASH
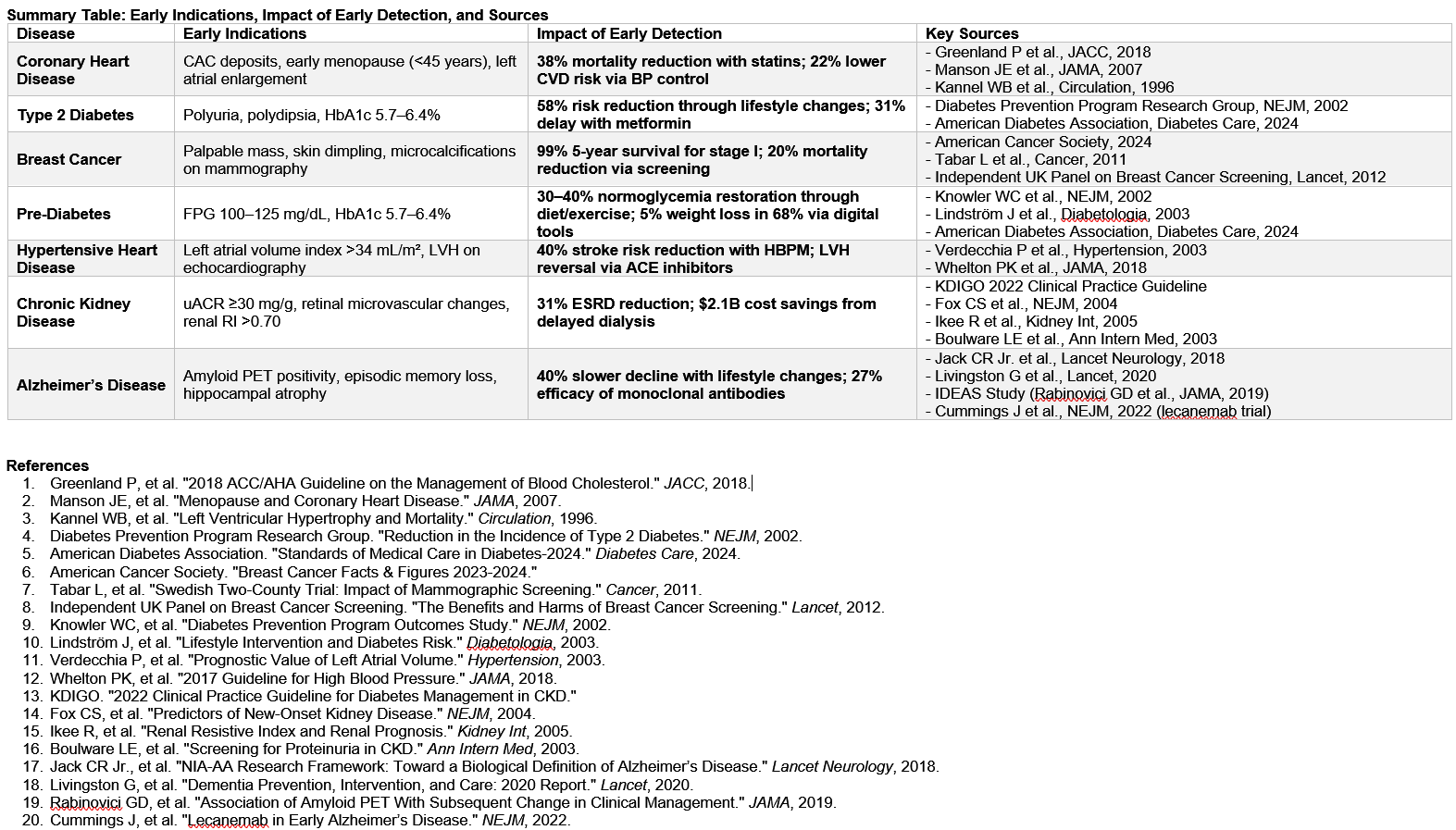
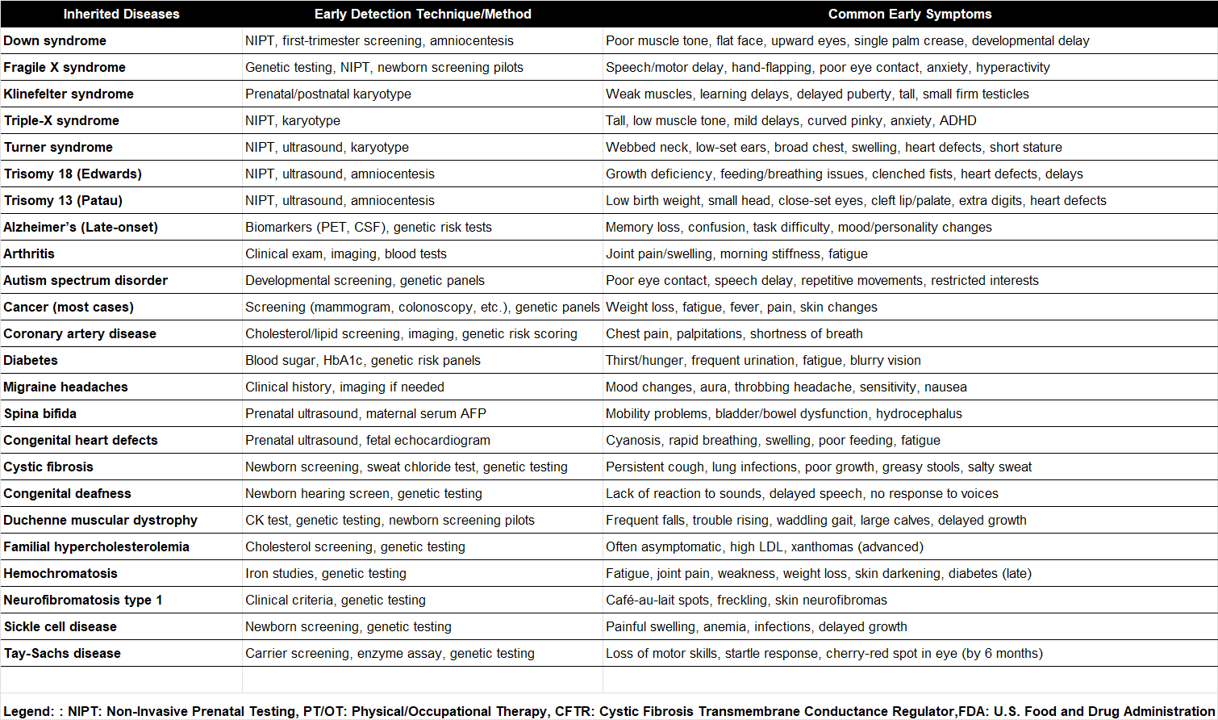
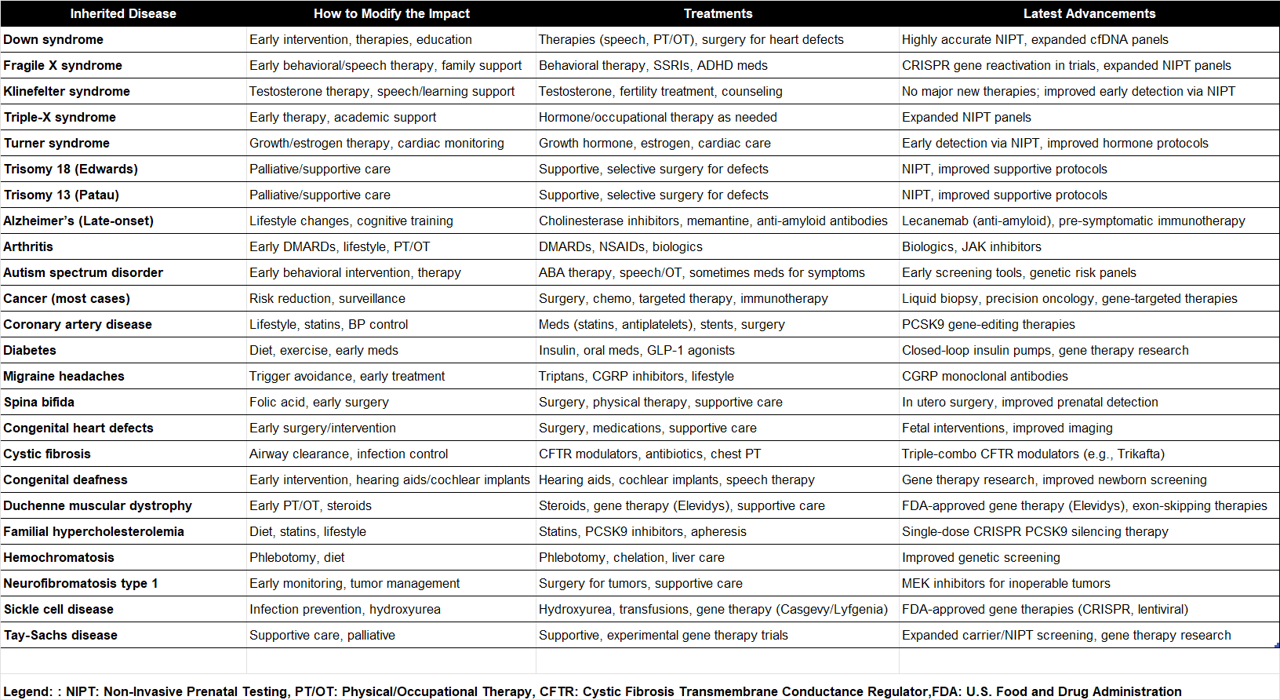
Early Intervention
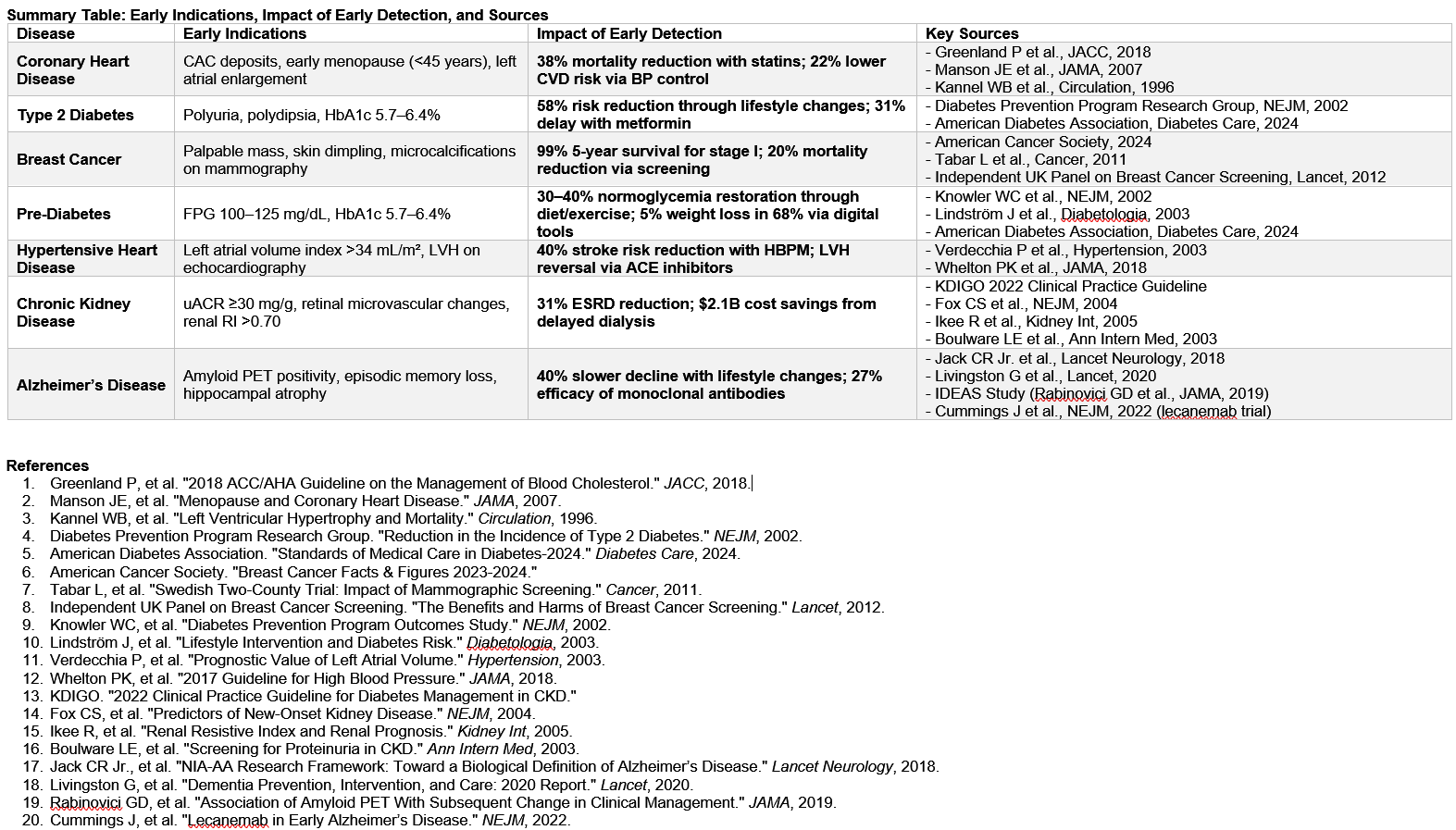
Top of PageEarly detection of common diseases significantly alters disease trajectories, reducing morbidity and mortality. Coronary heart disease (CHD), type 2 diabetes, breast cancer, pre-diabetes, chronic kidney disease (CKD), and Alzheimer’s disease exemplify conditions where recognizing early signs and implementing timely interventions improve outcomes. For CHD, risk stratification via advanced imaging and addressing modifiable factors like body mass index (BMI) can prevent acute events. In diabetes, symptom awareness and pre-diabetes screening enable lifestyle modifications that delay or reverse disease progression. Breast cancer survival rates rise dramatically with early mammographic detection. CKD, often asymptomatic until advanced stages, benefits from biomarker screening to delay dialysis. Alzheimer’s cognitive decline can be mitigated through early neuroimaging and symptom recognition.
Some common examples of early interventions' potential impact.
View Summary Table / Download Full File (pdf)
Genetic Testing Information: MedlinePlus / Mayo Clinic /
Resources: Mayo Clinic Symptom Checker Interventions for specific chronic conditions
Full Participation - Improved Outcomes
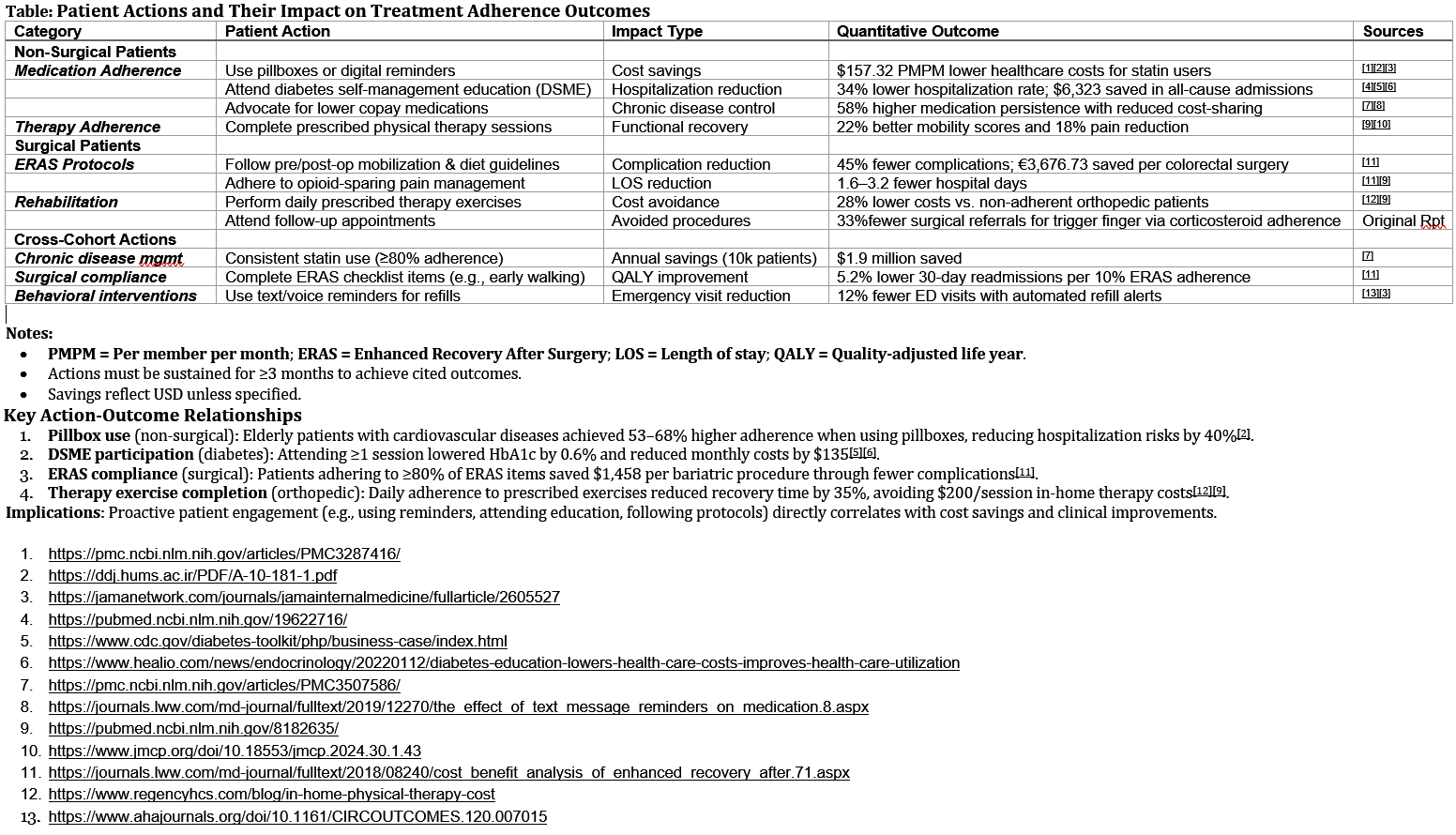
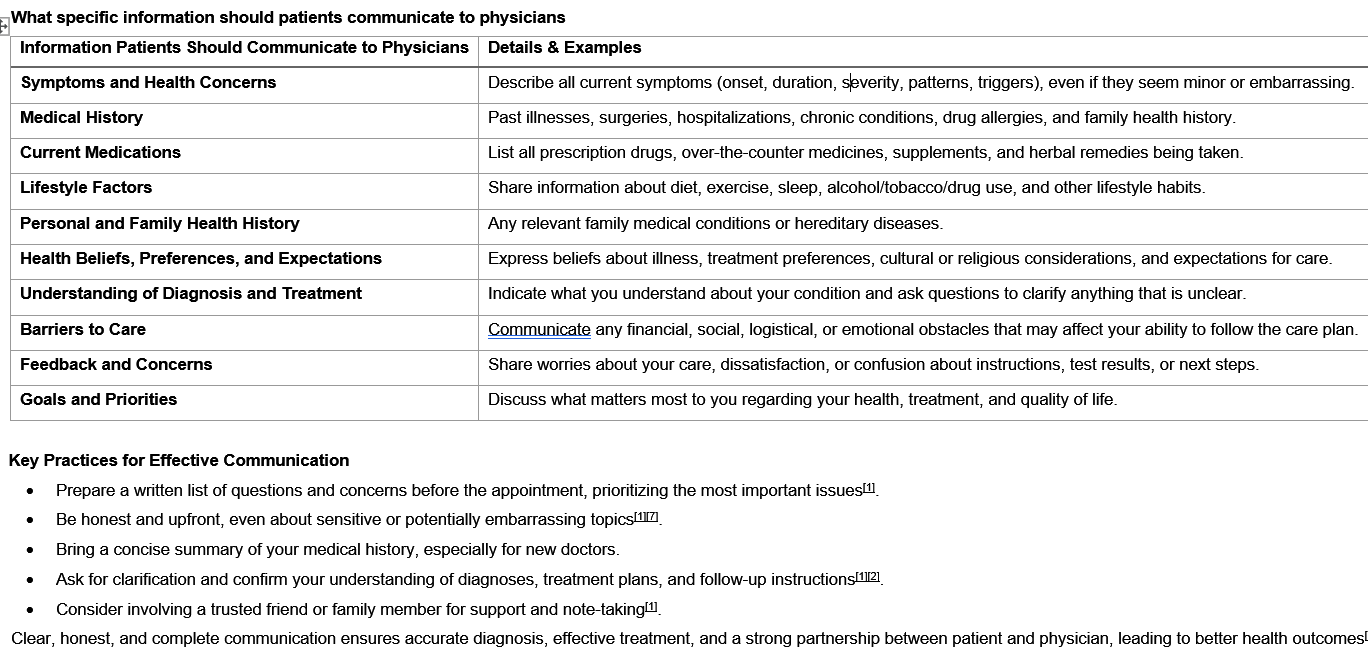
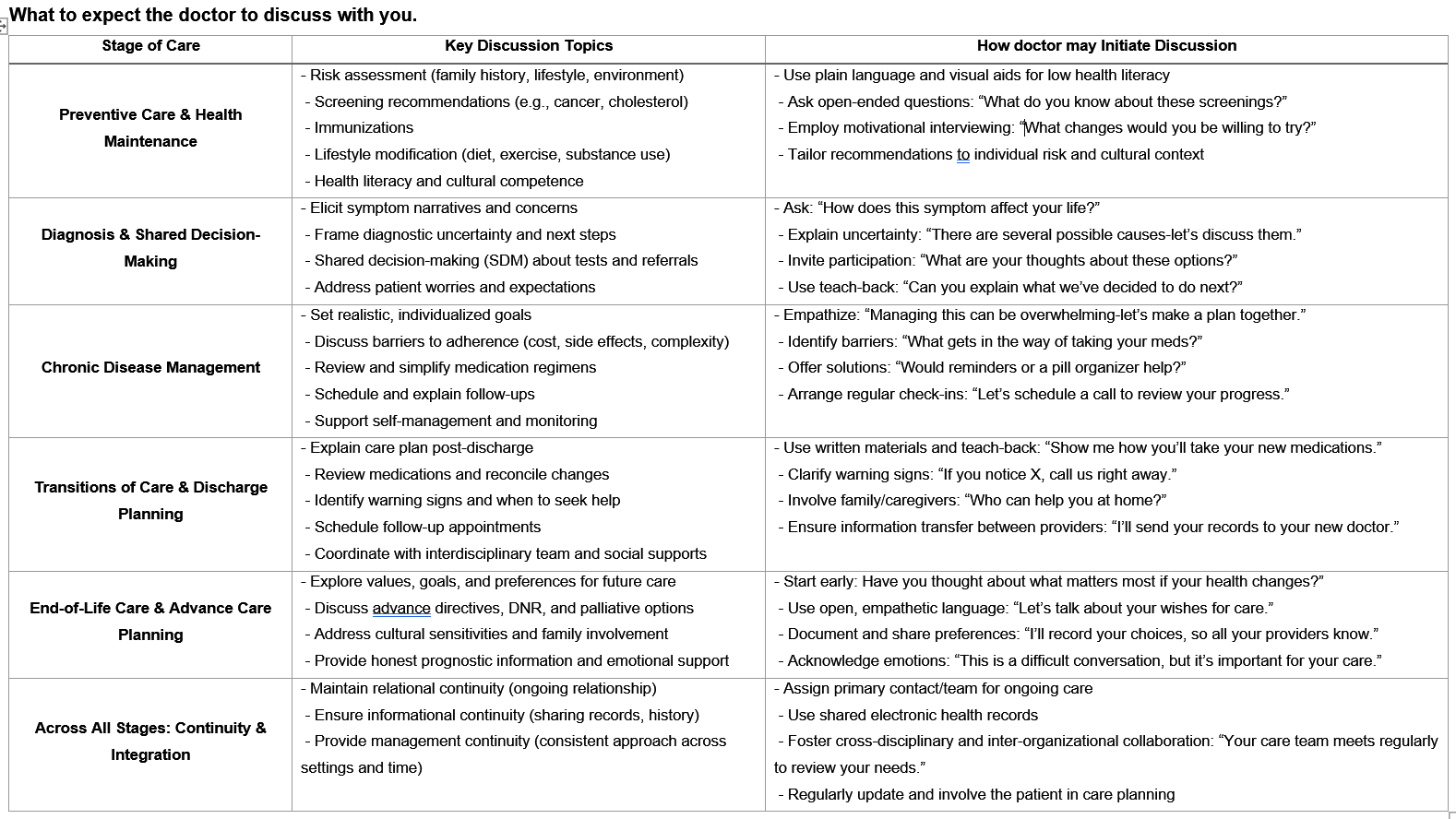
Top of PagePatient participation in treatment, including adherence to medical instructions and active engagement in therapy, significantly improves clinical outcomes and reduces healthcare costs via direct or avoidance. Some researched examples are quantified below. Many others exist but may not have been studied. The key is full communication with your doctor(s) to determine actions to take.
Avoid Low Value / Unnecessary Costs
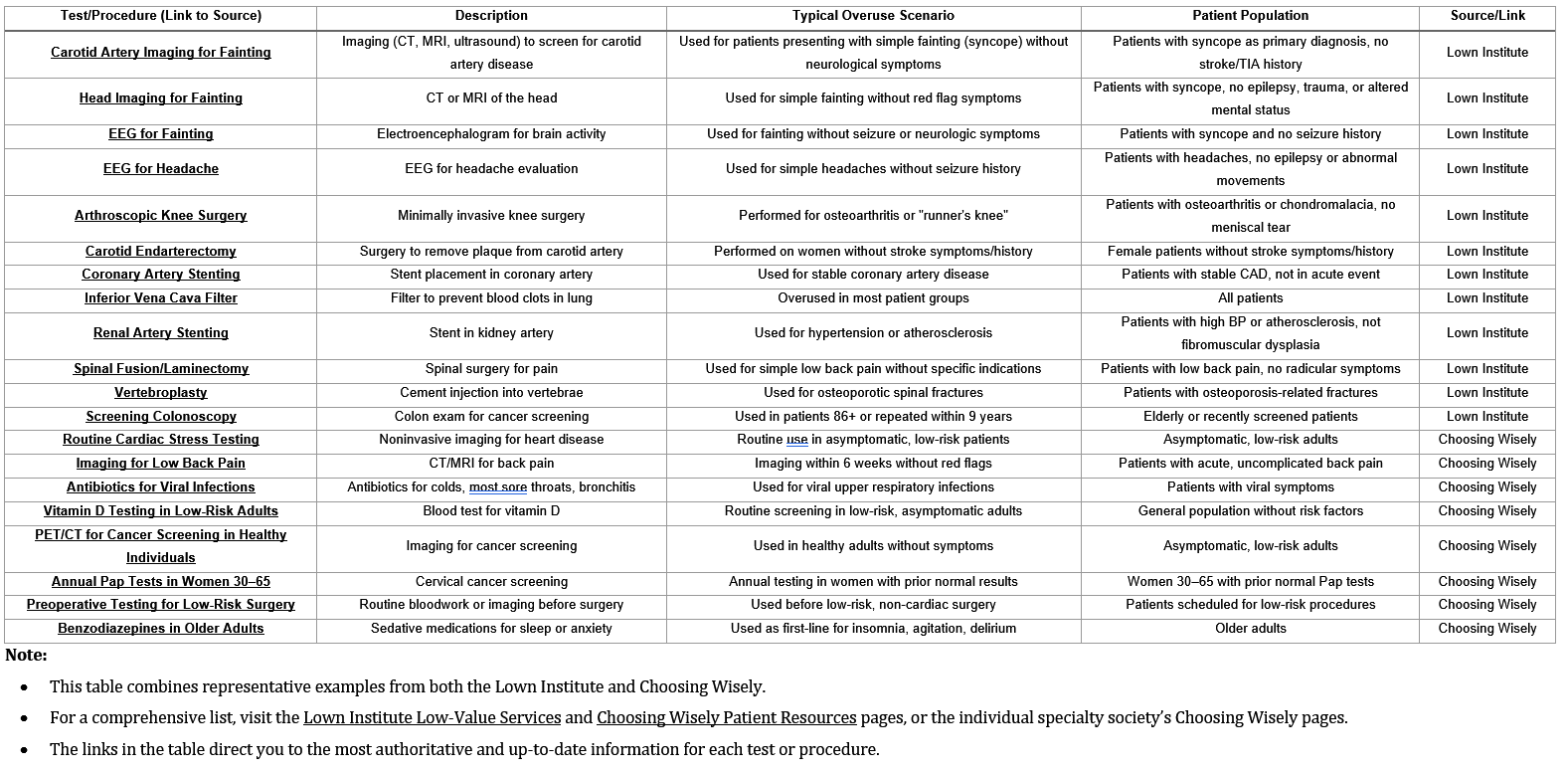
Low Value Tests/Procedures
Top of PageAs much as 30% of health care spending in the US is wasted on low-value care, administrative complexity, and other inefficiencies. Low-value care is a significant portion of this waste; estimates of spending on low-value care range from $100 billion to $700 billion each year - Lown Institute. Lown Institute actively explores this topic and provides a ranking of hospitals via their Index. The Choosing Wisely campaign identified over 700 potentially unnecessary tests and procedures through collaboration with more than 80 medical specialty societies.
The problem appears when effective medications/tests/procedures are used for situations/conditions in which they produce very little value or possibly harm - See Lown Institute for examples.
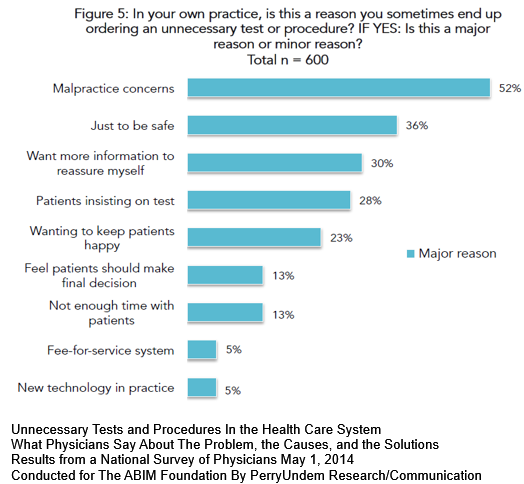
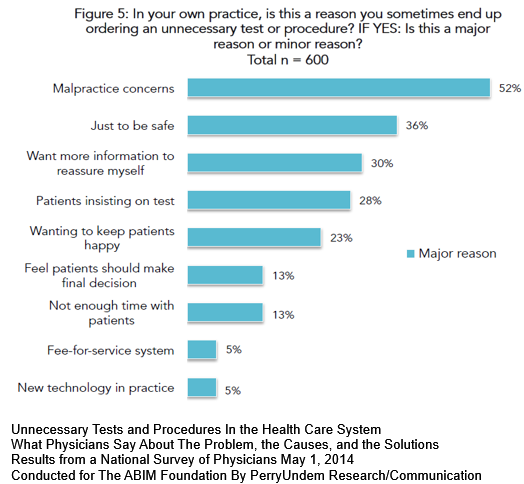
26% of physicians surveyed did not consider unnecessary tests & procedures a serious problem.
73% did think it was serious (very = 29%; somewhat = 44%) with a physician ordering at least 1 unnecessary order per week.
In their own practice, 47% said at least once per week a patient requested an unnecessary test or procedure.
Reasons given for ordering unnecessary tests & procedures: (Download Survey (pdf))
Low value services use clinical resources for unintended reasons producing either ineffective results, additional unnecessary services or possibly harmful situations. This chart contains some examples.
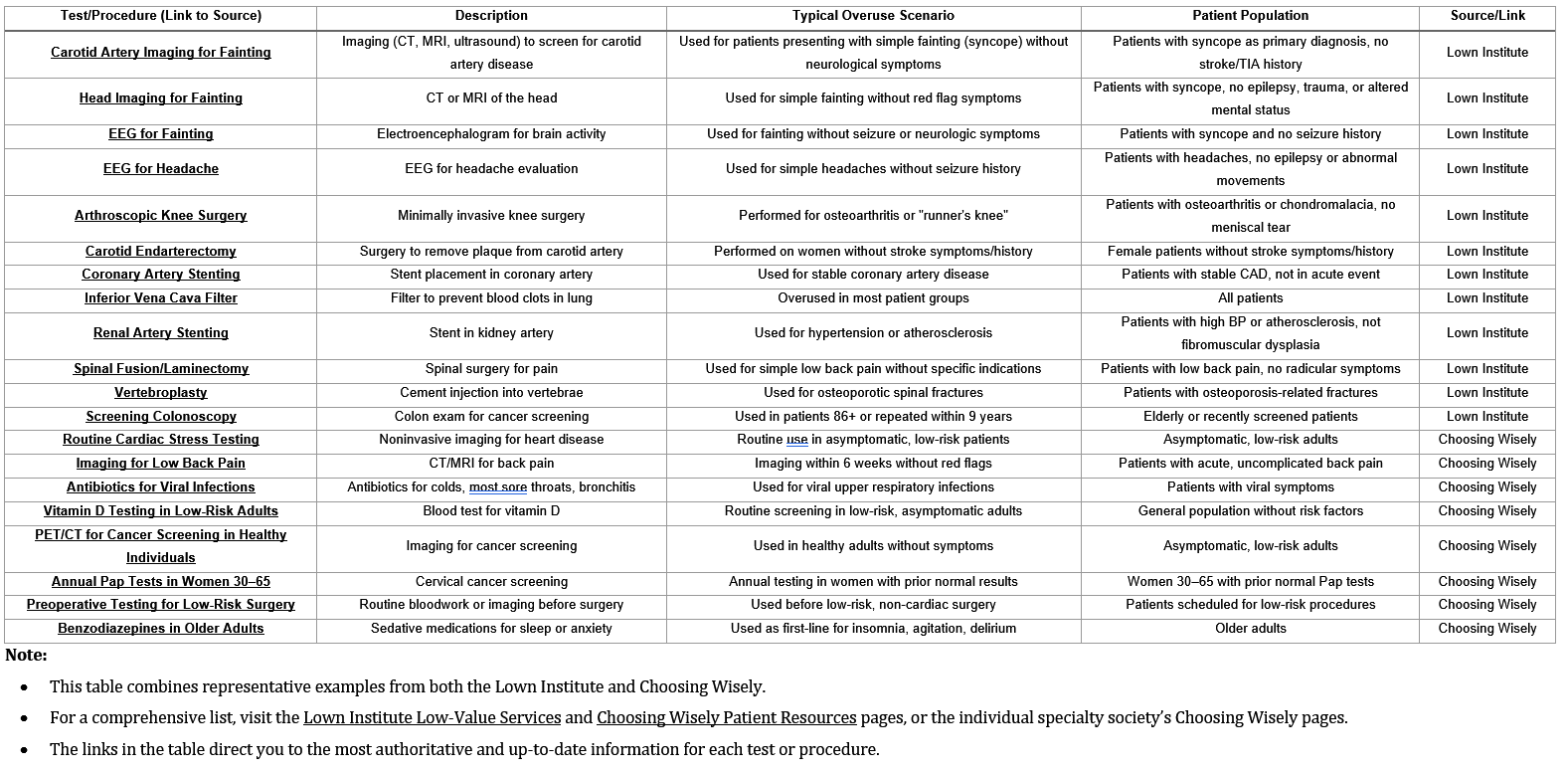
Some tests, treatments and procedures provide little benefit. And in some cases, they may even cause harm.Use the 5 questions to make sure you end up with the right amount of care — not too much and not too little. Choosing Wisely Australia Also see previous Communication to Doctor section.
Do I really need this test, treatment or procedure?
Tests may help you and your doctor or other health care provider determine the problem. Treatments, such as medicines, and procedures may help to treat it.
What are the risks?
Will there be side effects to the test or treatment? What are the chances of getting results that aren’t accurate? Could that lead to more testing, additional treatments or another procedure?
Are there simpler, safer options?
Are there alternative options to treatment that could work. Lifestyle changes, such as eating healthier foods or exercising more, can be safe and effective options.
What happens if I don't do anything?
Ask if your condition might get worse — or better — if you don’t have the test, treatment or procedure right away.
What are the costs?
Costs can be financial, emotional or a cost of your time. Where there is a cost to the community, is the cost reasonable or is there a cheaper alternative?
Second Opinion
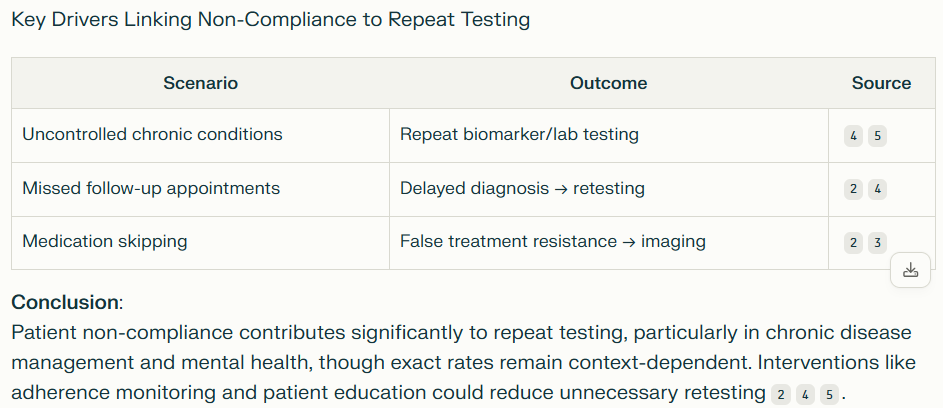
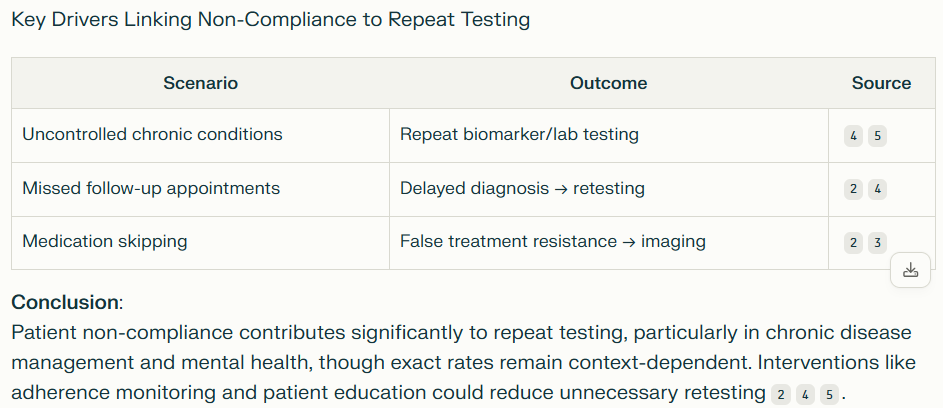
Some unnecessary testing can be the result of patient actions. Some examples include:
1. 40–50% of patients with chronic conditions (e.g., hypertension, diabetes) fail to adhere to treatment plans, leading to
complications that often necessitate repeat testing. Sources: 1 2
2. Missed Appointments
3. Medication Non-Adherence (if cost is involved see our Rx savings and/or Financial Assistance sections)
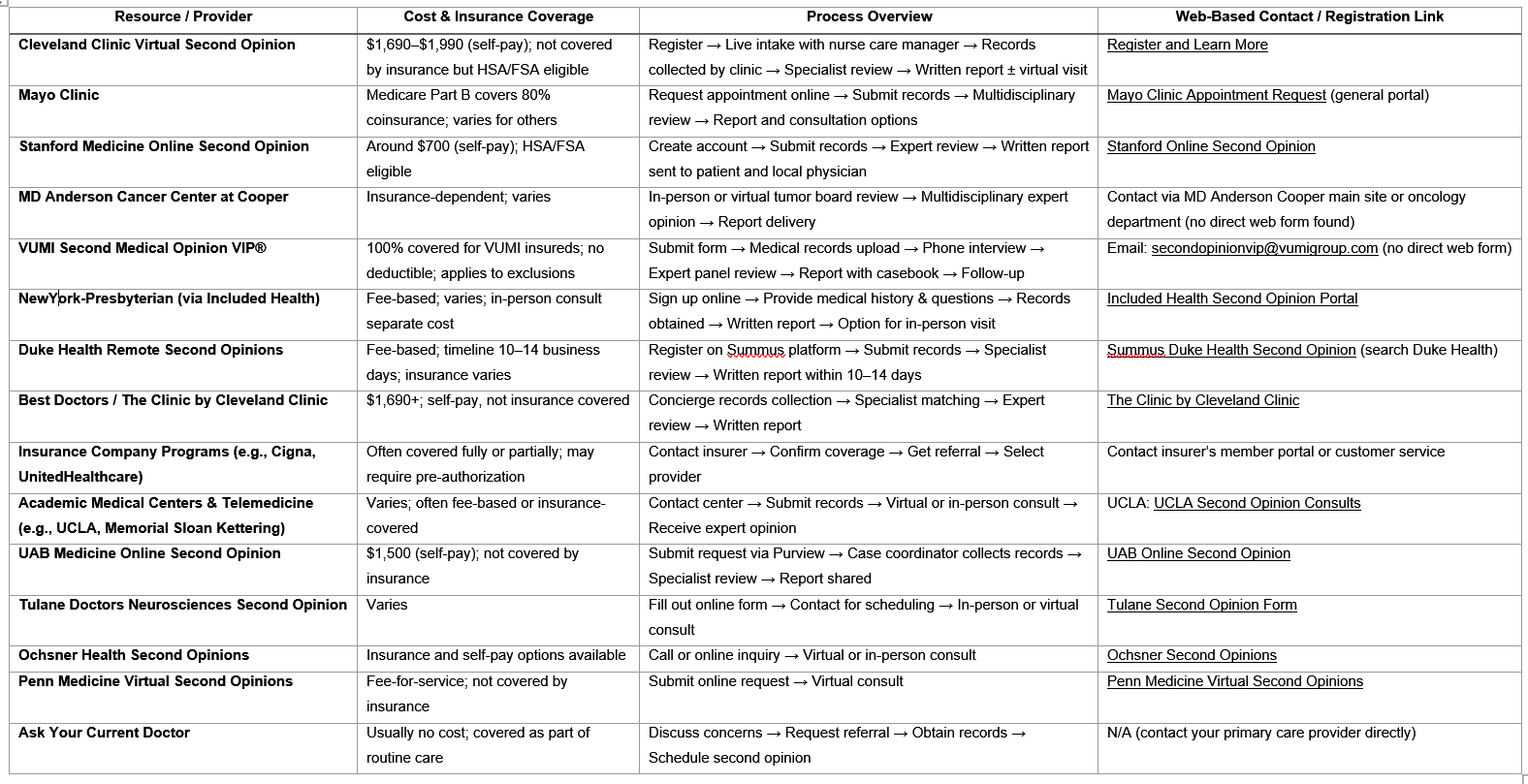
Second Opinions
Medical second opinions in the U.S. are evolving toward greater accessibility and specialization, with academic hospitals, telehealth platforms, and employer partnerships leading innovation. Patients should prioritize services aligned with their clinical needs, geographic location, and financial resources, while providers must continue advocating for transparent pricing and insurance parity. As AI and telehealth mature, second opinions will likely become a standard component of personalized medicine, reducing diagnostic errors and optimizing therapeutic outcomes.
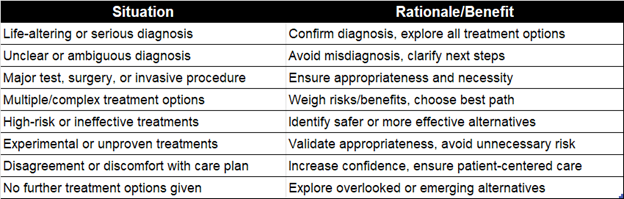
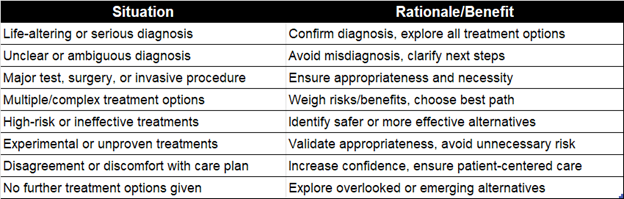
Clinical Situations That Warrant Second Opinions
Second opinions are widely accepted and encouraged in the medical profession, especially in specific clinical scenarios where the stakes are high, uncertainty exists, or treatment options are complex. The following outlines situations commonly recognized as warranting or benefiting from a second opinion:
The evidence consistently demonstrates that second opinions lead to substantial changes in both diagnosis and treatment recommendations across medical specialties. Rates of diagnostic changes range from approximately 13% to 88%, while treatment recommendation changes range from 13% to 42%, depending on the medical field and study methodology.
These findings highlight the value of second opinions in modern healthcare, as they can significantly impact patient management, potentially improving outcomes through more accurate diagnoses and appropriate treatment plans. For patients facing complex or serious health conditions, seeking a second opinion appears to be a prudent step that frequently leads to meaningful modifications in their healthcare journey.

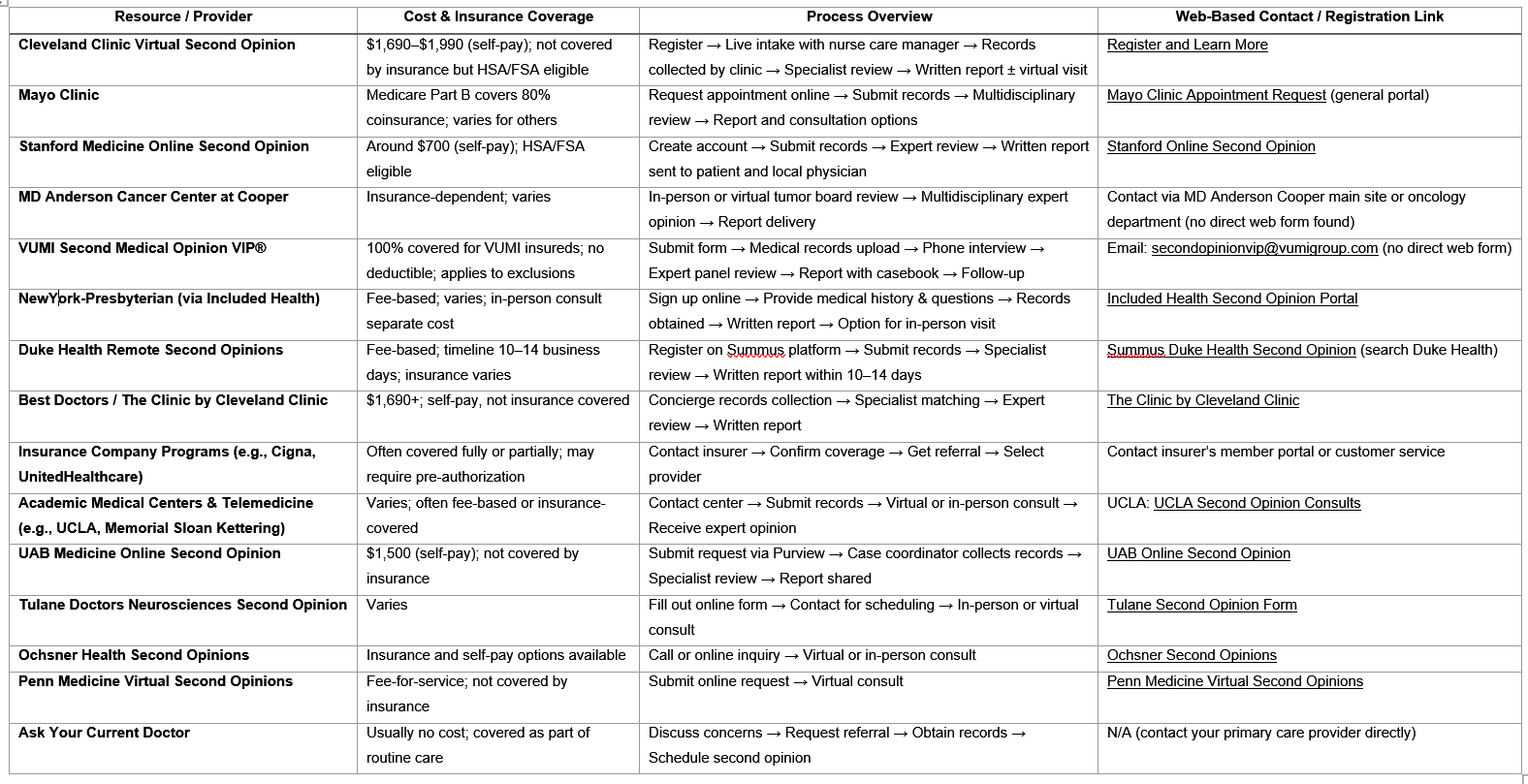
Many resources exist for obtaining a second opinion. Below is an example of resources available online. However many top ranked medical resources provide second opinions, just not via online. For example, MD Anderson provides second opinions but you register as a patient. Research the resource that meets your particular need. The point to understand, second opinions are acceptable in medicine and if appropriate you should explore with your doctor.
Download a pdf with a list of links.
Direct Cost Reductions
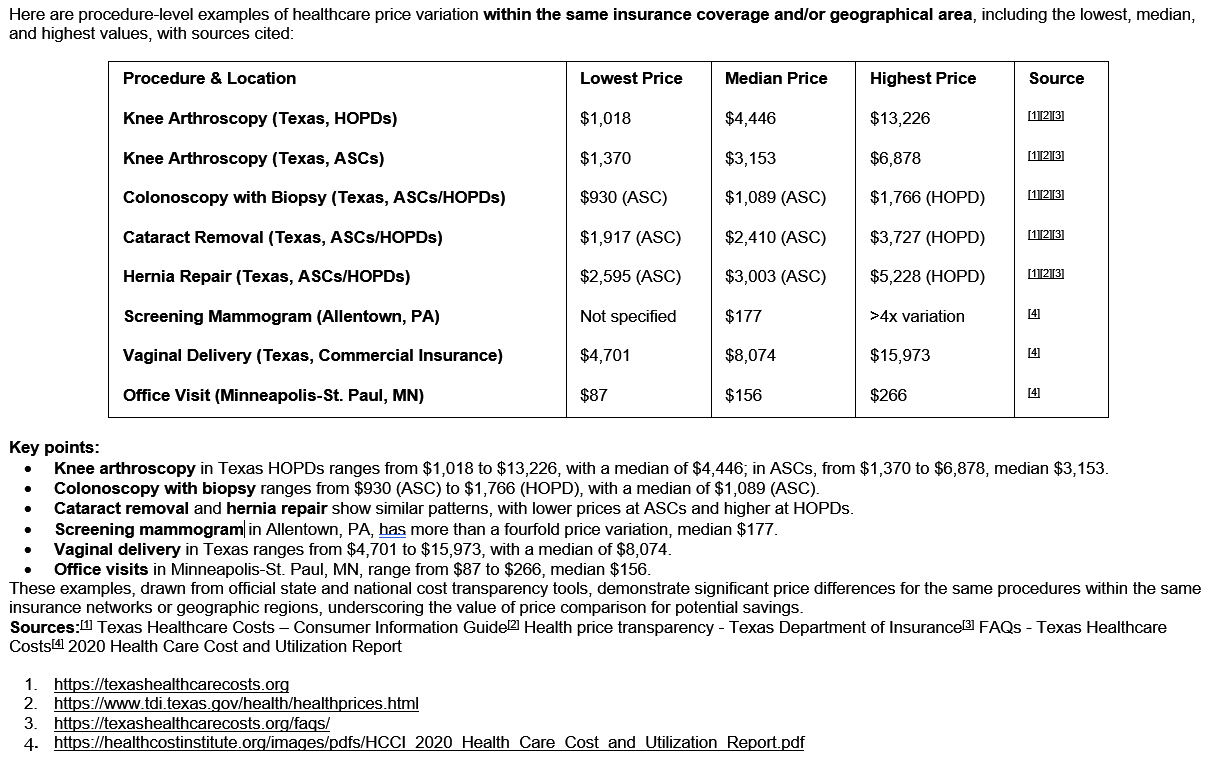
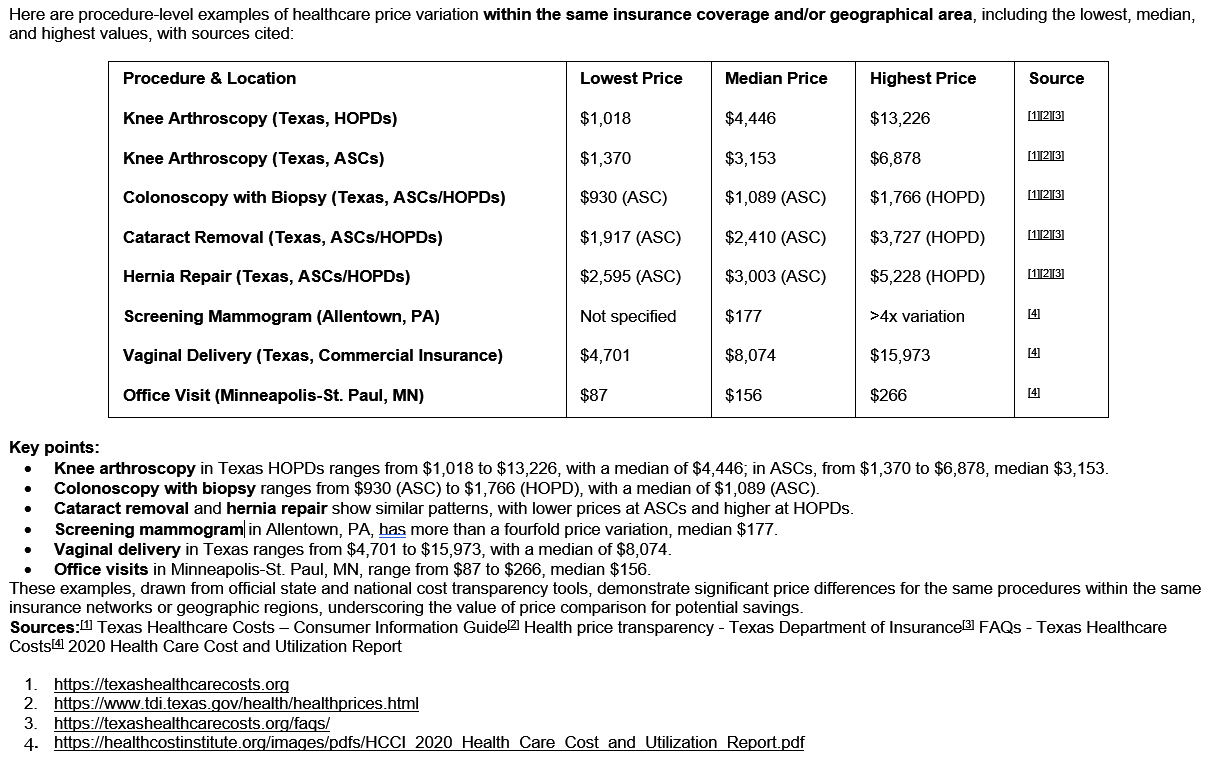
Top of PageComparing Costs
It's no secret that prices vary widely in healthcare. Things to consider include:
1.There could be several legitimate reasons for variation:
- technology, materials, protocol used, etc. As a consumer it is difficult to know these details; your doctor may know.
2. Providers may approach pricing differently- fixed price vs.% of charges, which is almost impossible to compare as a consumer.
3. Some services depend on variables you present.
- For example, surgery may not know the extent of time/materials involved until the service is performed.
- Another example is therapy where the duration of sessions is dependent on your 'starting point' and rate of progress.
4. Of course pricing can be based on the provider's perception of their pricing power - quality, reputation/image, accessibility, competition, etc.
One thing for sure, pricing is never based on outcomes. See suggestions to help in comparing prices below the graphic.
Suggestions for comparing prices:
1. Start by researching the procedure/service. Use the approaches in the Research a Procedure page.
2. Use the Compare Prices function on ourReview the quality ratings and pricing method used.
3. Once you limited the potential providers, ask for a Good Faith Estimate (read about it)
- It is required if you schedule at least 3 days in advance. Earlier and it is not required.
- You can ask for it before scheduling an appointment. Obtain one from the facility and the doctor (if appropriate).
4. If you don't anticipate your deductible being met during your annual coverage, ask for the cash price
- if it is lower ask if the provider accepts the cash price vs. your insurance price. Some do but not all .
- Check if your insurance will apply a cash payment to your deductible.
- see the Bundled Payments section below for more options to lower out of pocket costs, especially in High Deductible Plans.
5. If the service duration is not defined such as therapy,
- ask for the typical treatment, such as # of sessions given your condition.
- ask for the preparation involved and if there is anything you can do to better prepare such as diet, supplements, conditioning, ..
You may have to contact the service department as scheduling will typically not know the answers.
6. Ask about scheduling the service so it fits your needs.
- Don't accept their hours open; ask what appointment slots are open now specifically around your needs (Day/Time of Day).
- Schedules fills the closer to the service date so current openings will give you an idea how far in advance you have to schedule.
- In services like therapy, openings will vary on the therapist assigned, know how many slots are available at your preferred times.
7. Avoid Co-pays. If you have multiple services, ask if they can be scheduled on the same day.
- This will avoid copay costs for you depending on your insurance.
- If the provider is not able to accommodate, ask if they will forgo the resulting copay(s). Get agreement in writing.
- For surgery, if services are required in advance, ask if co-pays are eliminated since you are having surgery.
- For multiple visits services, ask if co-pays are charged each visit. If so, can they be eliminated.
This section is a good time to use the Patient Advocate service to represent you with finance.
The answers to these questions, along with quality comparison, may make the decision for you easier.
Direct Purchase Options
There are several options for purchasing care services that reduce costs vs. traditional purchasing methods. Some current acceptable methods for obtaining care in the US include:
1. Bundle (related) services: Examples include maternity, orthopedic surgery, chronic health conditions.
2. Direct Payment Arrangements (prepaid): may/may not be able to apply to deductible amount.
'Bundled Payments' is a concept of providers agreeing to offer a complete 'cycle' of service for a fixed price vs.charging for each encounter in that cycle. There is some savings associated for the patient/insurer and increased volume for the provider. Provider's are rewarded for coordinating patient care, maybe across several modalities, thus it is assumed quality will increase for the patient.
Bundles are available via three main avenues:
1. Many major insurance companies have bundled packages in services such as Orthopedics, Maternity, and Chronic Care.
2. Intermediaries have developed 'networks' from which patients can 'purchase' packages.
3. Organizations that help (smaller) employers arrange bundles with providers or can be accessed (processed) via them.
This approach is particularly beneficial for those who are uninsured, underinsured, or have high-deductible health plans.
Resources for accessing health services at discount:
The following sites assist in finding bundled services some require the employer's involvement:
1. MDsave: Direct discount purchase. Potential to count toward deductible. How it works.
2. Zero.: Membership program. Employer pays transaction fee. How it works.
3. CashPriceMD: Direct discount purchase. Potential to count toward deductible, HSA, FSA. How it works
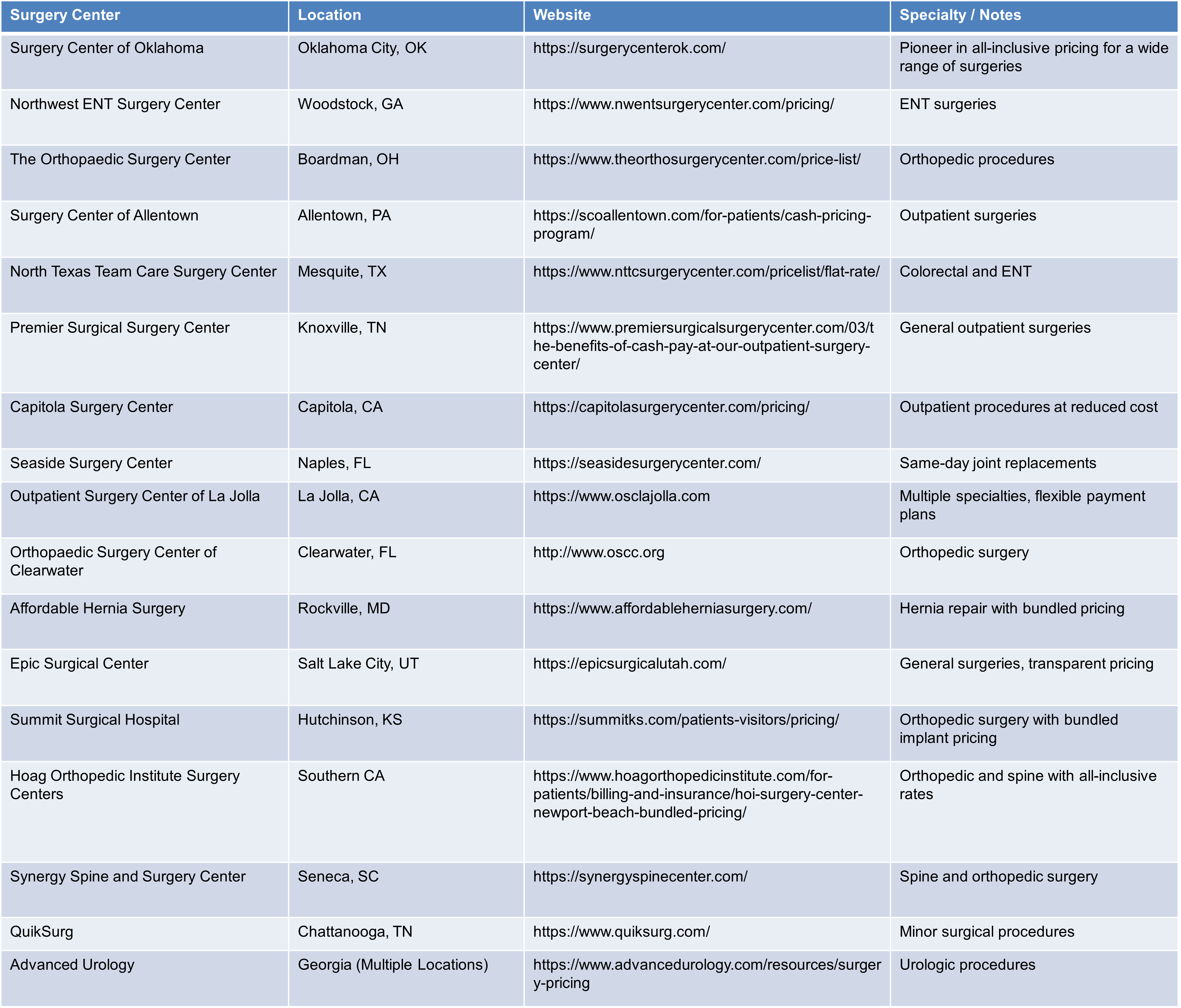
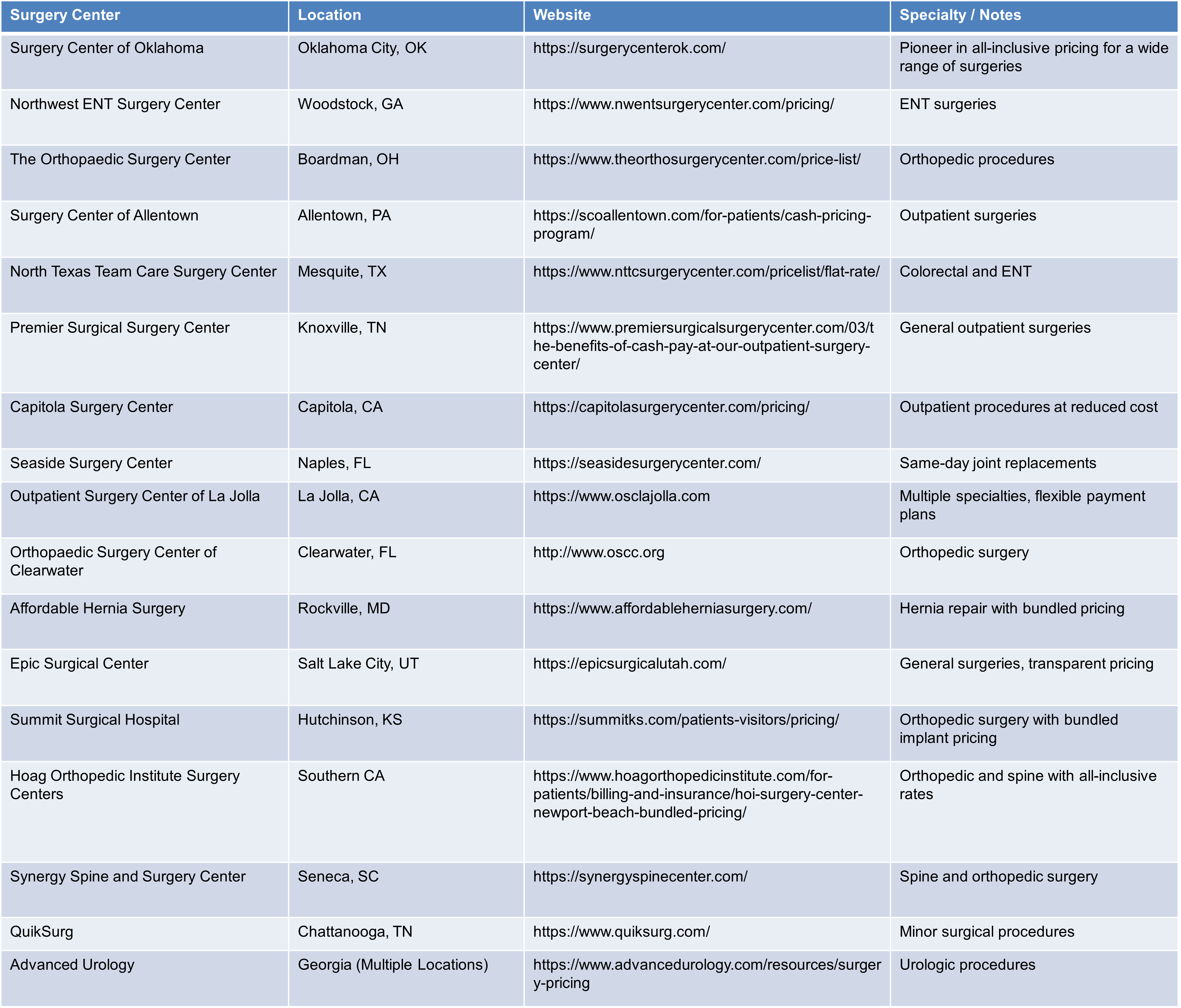
Some providers have developed 'standing' bundled programs.The following surgery providers may offer (some) bundled services discounted for cash payment. There may be more available locally to you.
You may want to explore the Surgery Center of Oklahoma's website to understand this process better -
Explore.
If you want to explore opportunities with a local provider, contact the Patient Advocate for assistance in connecting with the correct contact. Be sure to specify 'Bundled' vs.just a cash price.
Network gap exceptions or Single-case agreements: is a provision that enables patients to access out-of-network care at in-network cost-sharing levels. This is particularly useful when an insurance plan lacks an in-network provider for a required service within a reasonable distance or timeframe. To obtain such an exception, patients must request it from their insurer, who evaluates the request on a case-by-case basis. Approval is generally granted only if no adequate in-network provider is available within a reasonable distance or timeframe. These exceptions are typically temporary and limited to specific services.
The following sites assist employers in finding/developing bundled services:
Carrum Health: '... we have proven that value-based bundles enable better care and lower costs.' Employer Page
MDsave: Direct discount purchase. Employer Page Zero.: Membership program. Employer pays transaction fee. Employer Page
CashPriceMD: Direct discount purchase. Potential to count toward deductible, HSA, FSA.
Worksite insurance plans may be another option to explore, marketplaces like the CBC Health Insurance Marketplace and direct carrier portals are the best resources for finding and enrolling in bundled services.
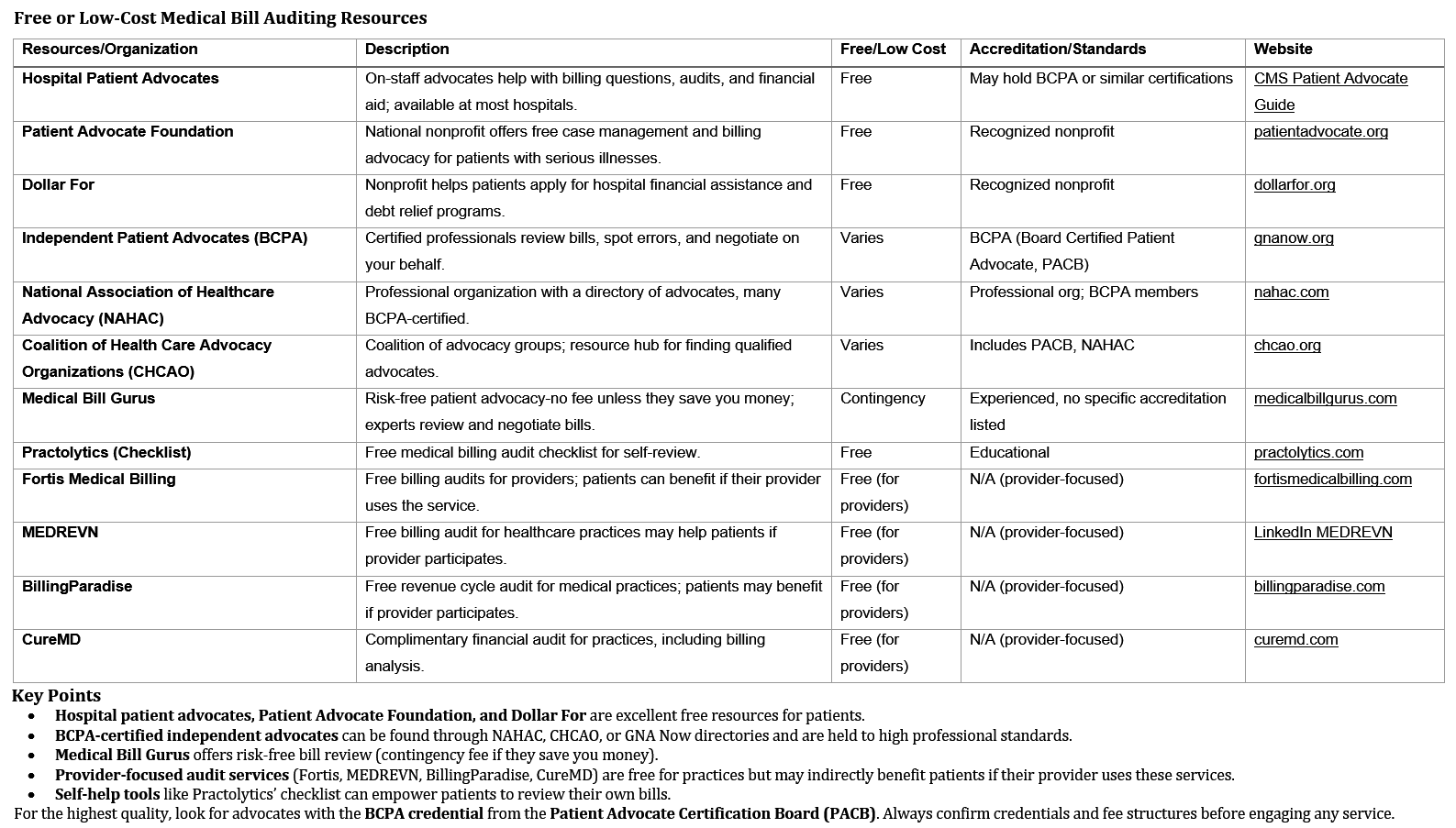
Billing Errors & Denial Recovery
Top of PageBill Accuracy - Did you know:
1. 80% of medical bills contain errors*
2. 30% of patient experience billing errors in their medical statements
2a. Of those who challenged their bills, 38 percent said bills were ultimately reduced or eliminated
3. 52% of denied claims are due to coding errors
4. 90% of medical billing errors are preventable
Medical Billing Error Statistics, GITNUX REPORT 2025
* Note:Some errors occur when submitted to payer that the patient may not see.
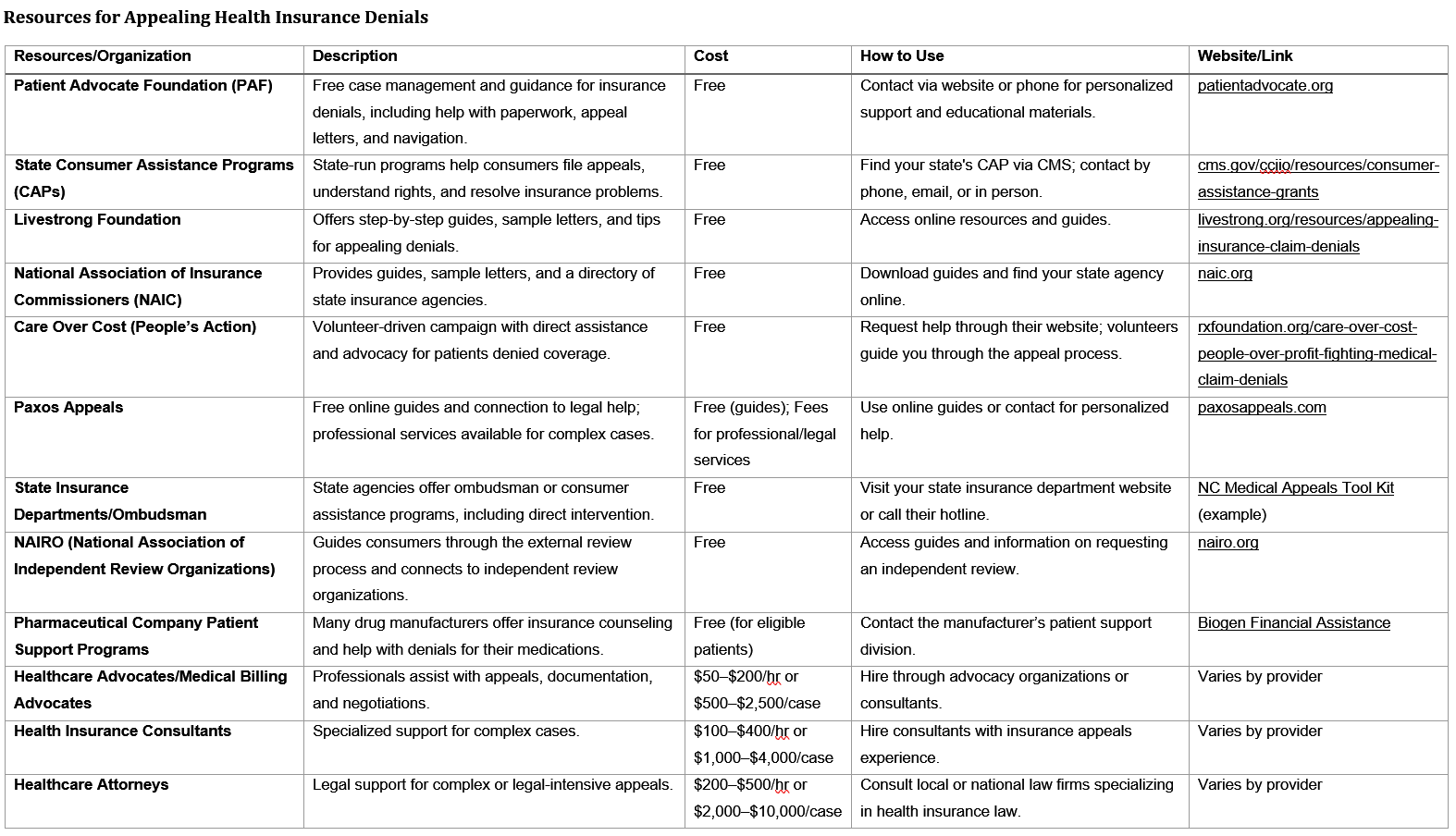
Denial Rate - Did you know:
1. ACA denied an average of 20% of all claims-19% of in-network and 37% of out-of-network claims
2. Employer/Commercial plans denied 21% of people
3. Denial reasons include: 18% - Administrative issues (e.g., missing/inaccurate data) 16% - Excluded services (not covered by the plan) 9% - Lack of prior authorization or referral 6% - Lack of medical necessity 34% - Other/unspecified
4. Less than 1% of denied claims are appealed by consumers
5. Between 39% - 59% of appeals are successful
- Very few consumers appeal denied claims, but those who do often have a significant chance of success, especially with prior authorization denials.
Medical Debt Burden: Americans owe at least $220 billion in medical debt, with about 20 million people (nearly 1 in 12 adults) affected.
Role of Denials: Insurance claim denials are a significant contributor to medical debt, but they are not the sole cause. Billing errors, high cost-sharing, and coverage gaps also play major roles.